
Osteochondrosis of the cervical spine or cervical osteochondrosis is a disease of degenerative-dystrophic genesis that affects the intervertebral discs and cervical vertebrae with the formation of protrusions and intervertebral hernias, which eventually leads to dysfunction of the spinal cord and is often the cause of patients. disability.
Features of the structure of the cervical spine
The vertebrae are the bones from which the spinal column is built. Each vertebra has a body that carries the entire load, the arch of the vertebrae, the transverse and spinous extensions.

The vertebral arches form the vertebral canal through which the spinal cord passes. Spinal processes are designed to strengthen the muscles of the back.
There are both anterior and posterior ligaments that connect the vertebrae to each other.
The intervertebral disc is a rounded flat structure consisting of annulus fibrosus and nucleus pulposus, whose main function is shock absorption. The intervertebral discs are located between the vertebrae.
The facet joint is a movable joint of two adjacent vertebrae. Facet joints provide flexibility to the spine.
The intervertebral foramen are openings formed by the structural elements (legs, joint extensions) of two adjacent vertebrae and are intended for the exit of the radicular nerves of the spinal cord.
There are paravertebral muscles that support the spine and its various movements.
The cervical spine is the uppermost and most mobile part of the spine, which consists of seven vertebrae and has a C shape due to forward bending (cervical lordosis).
All movements of the head - tilt, turn, circular, are provided by this part of the spine.
Interesting!In addition, the cervical spine is the most traumatized part, because the cervical vertebrae have weak strength and a weak muscular apparatus in relation to others.
Osteochondrosis of the cervical spine often occurs for the same reason.
Prevalence of cervical osteochondrosis
Osteochondrosis of the cervical spine affects the working-age population older than 30 years. This disease is more common in women than in men.
According to the World Health Organization, 40-90% of the world's population suffers from osteochondrosis.
Bitan!Every other patient with osteochondrosis has dystrophic and degenerative changes in the spine in the cervical spine.
Causes of osteochondrosis of the cervical spine
Osteochondrosis can be called a recognition of a person’s ability to stand and walk on two legs. This opinion is confirmed by the fact that no animal that walks on four legs suffers from osteochondrosis.
Despite the availability of modern methods for diagnosing the disease and a deep knowledge of human anatomy and physiology, it is still not possible to determine the specific causes of osteochondrosis.

But reliable factors are known that lead to degenerative-dystrophic changes in the spinal column. This includes the following:
- insufficiently mobile lifestyle of the person, which leads to weakening of the muscular apparatus of the back. Often office workers, cashiers, salespeople and drivers suffer from osteochondrosis;
- hard physical work;
- mechanical back injury;
- genetic predisposition to osteochondrosis;
- overweight and obesity;
- neuropsychiatric stress;
- improper workouts in the gym;
- beriberi, micronutrient deficiency, metabolic disorders;
- improper diet;
- the presence of diseases of the kidneys, digestive and endocrine systems;
- infectious diseases;
- frequent hypothermia of the body;
- congenital and acquired immunodeficiencies.
Pathogenesis (mechanism of development) of cervical osteochondrosis

Almost all factors that contribute to the development of osteochondrosis lead to back muscle spasm. In turn, muscle spasm disrupts the blood supply and bone metabolism of the vertebrae and intervertebral discs.
Thus, dystrophic changes occur, ie dehydration, dehydration and loss of elasticity of the vertebrae and intervertebral discs.
Further stress on the spine leads to flattening, protrusion (protrusion outside the annulus fibrosus) of the intervertebral discs.
No less important in the pathogenesis of cervical osteochondrosis is the load of holding and moving the head.
The load on the cervical vertebrae is huge, because the average weight of the head is 3-5 kg, and their bone tissue is, unfortunately, fragile and thin.
Also, the development of osteochondrosis has been facilitated by technical advances - smartphones, tablets, e-books, if you bend over while using these gadgets.
Intervertebral discs cannot efficiently perform spinal cushioning, so compensatory mechanisms are activated.
Bitan!One of these mechanisms is osteophyte proliferation and the development of spondylosis.
False joints can also form along the posterior surface of the vertebrae of the cervical spine - uncovertebral arthrosis.
All these processes eventually lead to a reduction in cervical lordosis (hypolordosis), protrusions and intervertebral discs, which sooner or later become the main cause of a person's disability or require urgent surgical treatment.
The pathogenesis of cervical osteochondrosis can be divided into four phases:
- Onset of cervical instability;
- Formation of protrusion of intervertebral discs, reduction of intervertebral fissure, beginning of destruction of annulus fibrosus, which leads to pinching of nerves, which is manifested by neck pain;
- The annulus fibrosus is completely destroyed and the nucleus pulposus extends beyond its boundaries, so that an intervertebral hernia is formed and the spine is deformed;
- Disability phase. The vertebrae grow together. It is difficult for patients to move. Sometimes the condition can improve, but not for long.
Symptoms and syndromes of osteochondrosis of the cervical spine

The main symptoms of cervical osteochondrosis include the following:
- persistent neck pain of a pulsating or painful nature, which may extend to the occipital part of the head, eye sockets, ears, and shoulder girdle;
- pain in the upper limbs, which increases when moving;
- stiffness of movements of the upper limbs, violation of their sensitivity (tingling, tingling, numbness), weakening of muscle strength;
- morning stiffness in the neck;
- pain in the cervical spine when moving the head;
- periodic dizziness with cervical osteochondrosis, darkening of the eyes, loss of consciousness with sharp turns of the head;
- feeling of tinnitus;
- hearing and vision impairment;
- feeling numb and burning in the tongue;
- cardialgia (heart pain), sometimes cervical osteochondrosis is mistaken for acute coronary syndrome. The difference is in the lack of nitrate effect;
- due to microcirculation disorders and lack of oxygen in the tissue, connective tissue proliferation occurs in the cervical spine, the so-called
All symptoms of cervical osteochondrosis can be grouped into the following syndromes:

- reflex;
- radicular;
- radicular-vascular;
- spinal compression;
- cerebral.
Reflex syndrome consists of cervical pain - intense pain in the neck, due to which the patient is forced to fixate the head and tense the neck muscles.
Palpation of spinous processes, paravertebral points and intervertebral discs brings and / or intensifies pain.
Also, reflex syndrome is characterized by pain in the upper limbs, occipital or temporal parts of the head.
Radicular syndrome is a combination of sharp acute pain that intensifies with head movements and occurs by pinching nerves in the intervertebral foramen.
Radicular-vascular syndrome is characterized by vegetative-trophic disorders in the form of humeral-scapular periarthritis.
The patient is worried about pain in the shoulder joint, stiffness of movement, impaired skin sensitivity, swelling of the hand and wrist. Also, the patient cannot return his hands.
Spinal compression syndrome is caused by compression of the spinal cord and its vascular apparatus. Disc herniation, osteophytes, thickening of the yellow ligament can lead to this.
Interesting!Patients have pain in the cervico-shoulder region, flaccid paresis of the upper extremities and spastic paresis of the lower extremities, impaired sensitivity.
Cerebral syndrome with cervical osteochondrosis combines several such syndromes:
- diencephalic syndrome - increased irritability, neurasthenia, general weakness, insomnia, absence. In severe cases, there is anxiety, numbness of the upper and lower extremities, increased sweating, chills;
- posterior cervical sympathetic Barre's syndrome or "cervical migraine" - intense headaches, as in migraine in one half of the head on the background of dizziness, impaired vision and hearing, numbness in the hands.
- syncope syndrome - fainting with a sharp turn of the head;
- vestibular and cochlear tree syndromes - dizziness, gait instability, nausea, and even vomiting;
- visual disturbance syndrome - worsening of vision, visual disturbances, flickering of "spots", "flies" in front of the eyes.
Diagnosis of osteochondrosis of the cervical spine

Like any diagnosis in medicine, the diagnosis of osteochondrosis of the cervical spine is made on the basis of patient complaints, medical history, examination and auxiliary research methods.
In addition to the clinical examination, the patient must undergo the following methods:
- X-ray of the cervical spine;
- Computed tomography of the cervical spine;
- Magnetic resonance imaging of the cervical spine;
- Doppler ultrasound examination of the neck veins;
After diagnostic measures, the doctor chooses treatment tactics based on the results of diagnosis and analysis.
Treatment of osteochondrosis of the cervical spine
Treatment of osteochondrosis of the cervical spine consists in eliminating the radicular syndrome and eliminating the inflammatory process.

In the acute period of the disease, you must adhere to a strict bed rest. The soft mattress should be replaced with a hard one or a wooden shield should be placed over it.
Treatment of cervical osteochondrosis is carried out using the following groups of drugs:
- nonsteroidal anti-inflammatory drugs;
- chondroprotective drugs;
- painkillers and anti-inflammatory gels and ointments;
- vitamin preparations - ascorbic acid, retinol acetate, tocopherol acetate;
- calcium preparations;
- drugs that improve microcirculation in tissues;
- muscle relaxants.
Treatment of cervical osteochondrosis includes the following methods:
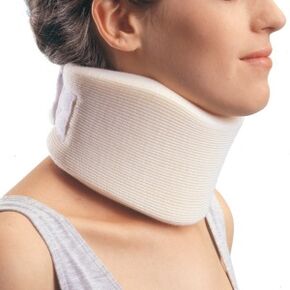
- wearing a special collar around the neck, which not only relieves the neck, but also restricts movement;
- stretching with a glisson loop - the patient's head, lying on the bed, is fixed with a glisson loop, and the head of the bed is raised by 20-30 cm. This procedure relaxes the muscular corset of the spine, increases intervertebral fissures, releases pinched nerves;
- manual therapy of cervical osteochondrosis should be performed only by an experienced manual therapist. Manual therapy is performed with the techniques of relaxing and segmental massage, mobilization which restores the damaged functions of the joints and manipulations to restore the full range of motion in the joints.
- physiotherapeutic methods for osteochondrosis of the cervical spine - diadynamic therapy, electrotherapy, laser therapy, shock wave therapy, balneotherapy, ultrasound and ultraviolet radiation treatment, magnetotherapy and other methods.
- Physiotherapy for cervical osteochondrosis includes exercises to strengthen the muscular corset. Physical activity is suitable not only for the treatment of osteochondrosis, but also for prevention. They can be done before bed at home, in the gym, at work and at school during breaks.
Surgical treatment of cervical osteochondrosis
Surgical treatment is indicated for severe radicular syndrome, which cannot be alleviated by medication, with increased impaired motor and sensory functions of the upper limbs, as well as with compression of the spinal cord.
Bitan!Operations to remove intervertebral disc herniation and osteophytes are widely used.
Prevention of osteochondrosis of the cervical spine

- healthy sleep on an orthopedic mattress;
- use of a low pillow;
- visit the sauna or bathtub regularly. The steam perfectly relaxes the neck muscles;
- you need to take a hot shower every day for at least 10 minutes;
- playing sports, gymnastics, walking. Swimming, yoga, pilates are great for this;
- all head movements should be precise, without sharp turns;
- properly distribute the load on the spine during physical work and sports;
- take breaks and warm up during sedentary work;
- maintain a proper position while sitting at a desk or computer;
- chairs and a table should suit your height.



















